A big cause for health concern
Arifun Nahar, 33, gave birth to her third child on December 16 through Cesarean section at a private hospital in the capital.
Upon health complications, doctors kept the baby in a Neonatal Intensive Care Unit and applied in the process almost all high antibiotics. As nothing worked, the newborn was shifted to the Dhaka Shishu (Children) Hospital where the baby boy eventually died 28 days after birth.
The cause of his sudden death was an otherwise harmless bacterium -- Klebsiella pneumoniae -- that turned deadly, possibly in hospital, by being resistant to 15 types of antibiotics.
“The baby developed infection of Klebsiella pneumoniae after birth; most probably from the NICU. This was one of the major causes behind his death,” Prof Samir K Saha, head of microbiology department at the Shishu Hospital, told The Daily Star.

For nearly a century, bacteria-fighting drugs known as antibiotics help control and destroy many of the harmful organisms that can make us sick. But in recent decades, overuse and misuse of antibiotics prompt some strains of bacteria to make a small change in their DNA and become antibiotic-resistant “superbugs”, experts say.
The World Health Organisation and researchers in developed world have long warned that “superbugs” are spreading rapidly due to the particularly high use of antibiotics in intensive care units, where patients are sickest and strong drugs are prescribed as routine.
And the latest data and analysis of Department of Microbiology and Immunology (DMI) at Bangabandhu Sheikh Mujib Medical University have reaffirmed that “superbugs”, like elsewhere in the world, are quietly becoming a big cause for concern in Bangladesh.
The largest data producer of bacterial and other infections in the country, DMI fears Bangladesh may experience a “disastrous situation” unless the “political leadership” takes bold steps immediately.
“Situation wasn't like this about 10 years back,” Prof Ahmed Abu Saleh, chairman of DMI, told The Daily Star. “About 70 percent of the deaths in ICUs are caused by AMR [antimicrobial resistance] infections.”
AMR is a situation when microorganisms like bacteria, virus and some parasites resist medicinal interventions.
“Basically, there is no new antibiotic in the pipeline for future use. At the same time, the available antibiotic drugs are losing their effectiveness -- which has made the scenario more dangerous,” he added.
Globally, some seven lakh people die each year due to AMR infections. The number of such deaths has been predicted to rise to 10 million by 2050 if things go unchecked, according to WHO.
There is no exact data about the number of deaths caused by AMR infections in Bangladesh.
However, a DMI laboratory analysis based on infections on patients' body from 2010 to 2018 depicted a sharp rise in the number of superbugs in Bangladesh.
In 2010, superbugs and multi-drug resistant (MDR) bacteria were detected in 6.5 percent cases. But it increased to 11-14 percent in 2018, according to the study.
“It is alarming because the percentage is increasing faster during the last one year than in the previous years,” said Ahmed Abu Saleh.
The microbiology department at Shishu Hospital analysed its own data of the same period (2010-2018). This data also showed existence of superbugs in around 11.3 percent of the tested microorganisms.
Besides, a Global Antibiotic Resistance Partnership (GARP) report titled “Antibiotic Use and Resistance in Bangladesh 2018” also stated that the rate of antibiotic resistance is growing in Bangladesh. But it didn't provide any quantitative data.
WHY AMR IN BANGLADESH
Use of counterfeit or poor quality of antimicrobial medicines, weak laboratory capacity, and inadequate drug monitoring and surveillance are among the main reasons behind the rise of AMR bacteria, the GARP report said.
Besides, the report said that poor treatment adherence, non-therapeutic use of antibiotics for growth promotion in farm animals, self-medication and over-the-counter access to antibiotics are to be blamed for AMR growth.
In Bangladesh, the size of the pharmaceutical market is worth Tk 22,000 crore. Of which, 18 percent is occupied by antibiotic drugs which indicates “indiscriminate use of antibiotic drugs”, Prof Sayedur Rahman, chairman of the Department of Pharmacology at BSMMU, told The Daily Star.
Also the lead researcher of the ongoing Antimicrobial Consumption Study under WHO, Rahman said, “We are gathering information. We will be able to say the actual consumption of antibiotic drugs within a few months.”
A 2015 study conducted by four Bangladeshi researchers on 1,500 patients showed that on average, 61.13 percent of the patients were prescribed antibiotics. Among them, around 33.80 percent were prescribed by unauthorised doctors. The European Journal of Scientific Research published the findings.
Inappropriate use of antimicrobials in livestock is also developing AMR bacteria which can be transferred through human contact with animals, Prof Saleh said, adding, “The biggest problem is that some 19 kinds of antibiotics are massively used in poultry and fisheries.”
A recent study conducted in Chattogram showed that some 54.55 percent of broiler birds (poultry chicken) were infected with multi-drug resistant bacteria.
The total number of livestock in the country is 393.14 million, according to department of livestock's data 2017-18.
WAY-OUT
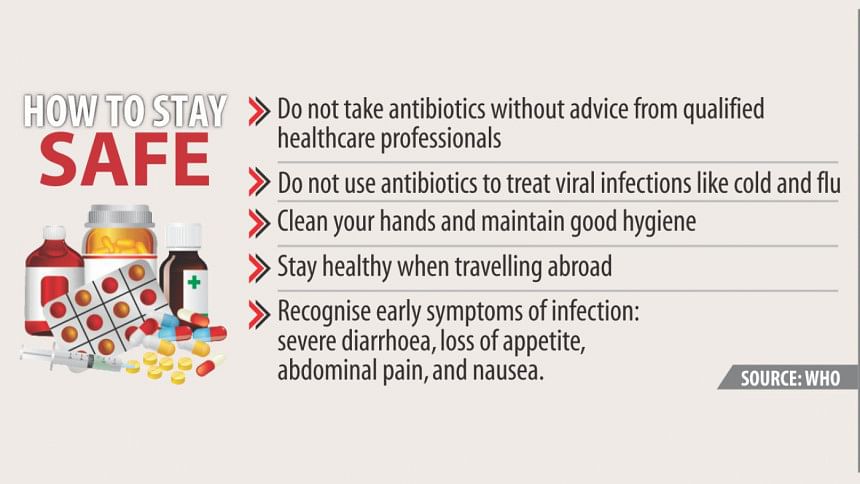
Experts have urged the government to take short- and long-term initiatives to control AMR. The measures include infection prevention and control, vaccination, antimicrobial stewardship, public and private practitioner education and a unified approach, namely one health approach across human and animal health.
Prof Sayedur said, “Firstly, over-the-counter sale of antibiotic drugs should be stopped immediately. Secondly, use of antibiotics in livestock sector, particularly poultry and fishery, should be controlled. Hand wash facilities should be initiated in all hospitals.
“There are no arrangements to test antimicrobial sensitivity in over 50 districts. For this, doctors start from comparatively high antibiotics based on their assumption. But they should not do this.”
The government should focus on the issue as the entire health system, including modern facilities and hygiene maintenance of the hospitals, is linked to it.
Pharmaceutical companies have also responsibilities in this regard. Many of them pressurise their representatives to boost sale of high antibiotics, which is wrong, he added.
Prof Saleh said, “Stopping the misuse of antibiotics is a matter of the government. We, the doctors, have very little to do in this regard, unless the government formulates a national policy and implements it … But it must be controlled.”

 For all latest news, follow The Daily Star's Google News channel.
For all latest news, follow The Daily Star's Google News channel. 






Comments