Covid-19 testing and health sector resource mobilisation
There has been a consistent plea from experts for ramping up the test numbers and testing capacity since the early stages of Covid-19 outbreak in Bangladesh. Currently, 77 PCR labs are in operation, which was only six at the end of March. Testing capacities have increased over time but are we doing enough?
If we consider the "positive rate"—the proportion of tested individuals returning a positive result—it has been 22-25 percent during the last several weeks. This means that out of 4-5 tests one person is found Covid-19 positive. According to the World Health Organization (WHO), a positive test rate between 3-12 percent is indicative of sufficient testing.
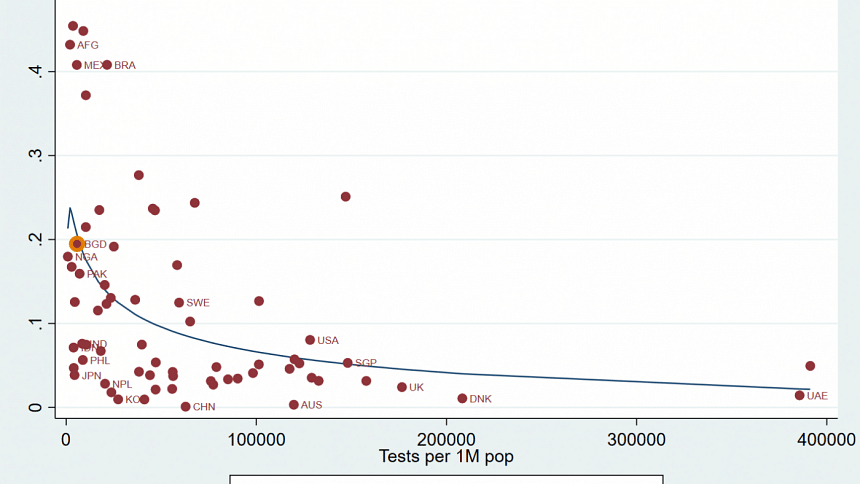
When we plot positive rates against the tests per million people of the 68 countries, it is evident that the positive rate drops drastically with the rise of test number. This evidence reinforces that the two important aspects of the Covid-19 crisis, testing and containment are closely linked.
Evidence from other countries also gives a better idea of whether a level of testing is sufficient for a country or not. For example, China did far less testing than the USA (8.04 percent) or UK (2.42 percent), but it seems enough for them as the positive rate in China is the lowest (0.09 percent). On the contrary, Brazil (40.81 percent) or Mexico (40.80 percent) are doing fewer tests with high positive rates, which indicates insufficient testing. Bangladesh has a low level of testing (146thposition in the world as per test/million) but significantly high positive rates. Many countries in Asia such as Japan (3.85 percent), Philippines (5.65 percent), India (7.59 percent) have similar levels of testing, but they have significantly lower positive rates. Clearly, testing status in Bangladesh indicates that we are yet to reach a enough level of testing to be able to have a close-to-reality picture of the spread of Covid-19.
Do we need more testing?
The importance of consistently testing more and more people to contain Covid-19 cannot be overemphasised. Adequate testing gives a true picture of infection and facilitates the subsequent measures that are of equal importance in ameliorating the crisis. Insufficient level of testing makes it difficult to: i) identify infected individuals and their locations; ii) trace their close contacts; iii) containment of infection by quarantining infected individuals and providing medical support if required; and iv) and isolate others who may have come in contact with infected individuals.
This brings us to the second aspect of our analysis where we found that some countries did better in terms of positive rates even after the spread of the virus by an effective testing policy. If we examine the daily growth of Covid-19 cases and test numbers, and the trend of positive rate from April to July, an alarming scenario is evident about Bangladesh. When the countries increase the test growth aggressively and effectively the infection rate goes down and eventually, it reduces the growth of Covid-19 cases. However, the countries that failed to do so, the infection grows dramatically e.g. Mexico or Brazil. In other words, the infection rate should go down gradually if there is enough testing.
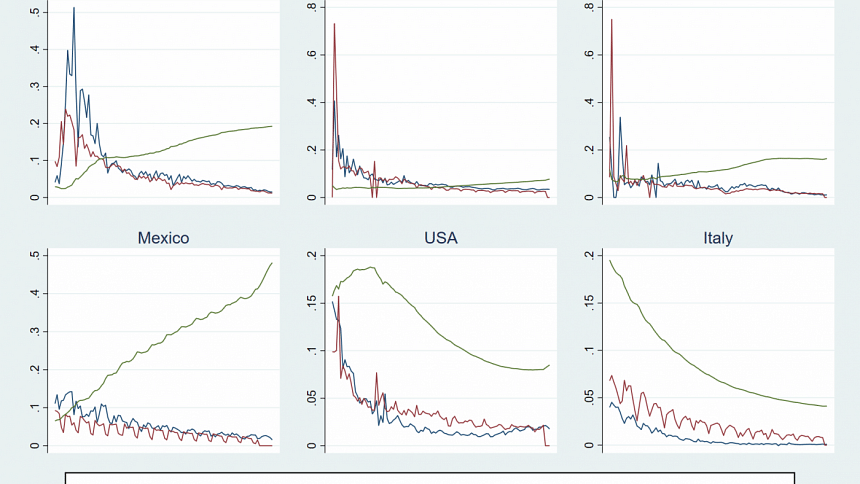
While this evidence is not novel, they reinforce the necessity of carrying out tests at a consistently high rate along with thorough and systematic contact-tracing and strict implementation of quarantine, isolating, and other protective measures. Yet, the number of tests performed daily has been dropping consistently.
The number of daily tests has dropped by 4,613 between July 8-12, amidst concerns of the rapid spread of the deadly virus and this lower testing has contributed to the rise in positive rate, which is 24.95 percent as of July 13. That indicates, like the cross-country analysis, there is no room to reduce tests with upward trending positive rates.
Health budget: Where are we heading in testing and curing?
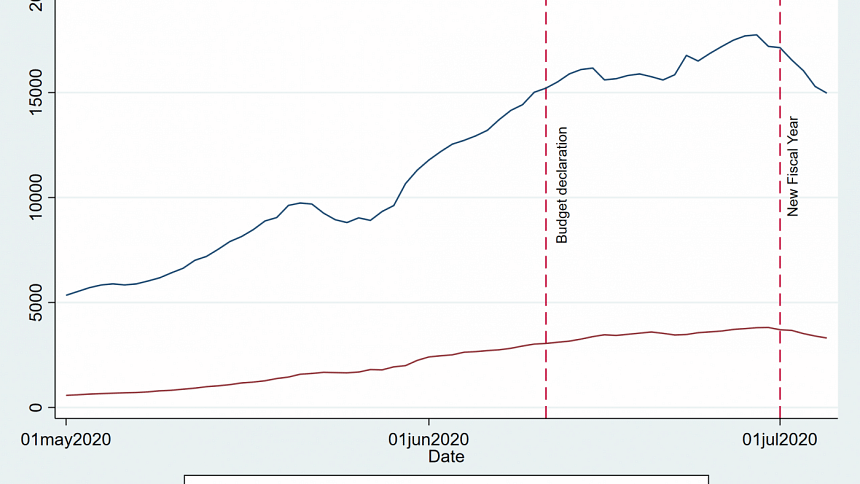
Indeed, response to Covid-19 pandemic, including testing, varied to a large extent by the fiscal condition of countries. Prolonged lockdown, massive income losses experienced by millions, and most importantly, a fragile public health system had created additional interest in and shaped the expectation of the people from the budget for the fiscal year 2020-2021. The general expectation was to see extensive allocation in all possible frontiers e.g. health, safety nets, education, etc. for battling Covid-19 impacts. How far the budget has addressed our expectations, however, remains a big question.
Broadly, the government allocated 5.2 percent (Tk 29,247 crores) of its total budget in the health sector this year. The health sector had been receiving similar allocation in the last decade—average allocation in the sector is 5.1 percent of total fiscal expenditure. So, the allocation remains more or less the same, with only an insignificant increase from the average allocation in the last decade. The provision of funds in the current fiscal year represents an increase of 13.66 percent from the previous FY, which was 10.1 percent in the budget of FY2019-20. Thus, allocation to the health sector increased by only 3.5 percentage points in the 2020-21 budget.
In all sectoral allocation, there are two components: recurrent and capital expenditure. Recurrent expenditures include all day to day operational expenses whereas capital expenditures include the infrastructure and facility improvement related expenses. In FY2020-21 budget, the allocation for recurrent expenditure increased by 22.82 percent while the allocation for capital expenditure decreased by 0.96 percent. Understandably, the increase in day to day expenditures has been driven by the high pressure in the public hospital system. However, enhancing health care facilities is also critical, for both short-term and long-term use to fight against this pandemic, which is surprisingly absent, rather lowered.
In the recurrent expenditure of health services, the highest growth (32.15 percent) occurs in wages and salaries, perhaps to meet the additional expenses for salaries and wages due to recruiting more doctors and nurses. However, the budgetary allocation of medical supplies has not increased noticeably compared to the previous FY. It increased by 11.23 percent in FY2020-21 from 2019-20, whereas the increase was 15.08 percent in 2019-20 budget from FY2018-19. It raises a concern about testing capacity, stock of personal protective equipment, and provision for lifesaving drugs for poorer patients.
After the budget, we also observe the imposition of a fee for the test which applies to the poor and rich equally. Even if people were ready to pay, they had to wait in queue for up to 12 hours to be tested. Moreover, the Directorate General of Drug Administration, the apex body for approving drugs and testing kits, is one of the core divisions of the health sector. The need for resources to try new drugs, vaccines, and testing kits are paramount. However, the proposed budget does not speak to that need.
In the budget speech, it has been declared a lump sum allocation of Tk 10,000 crore to fight against Covid-19. However, it is not clear how this amount will be allocated to meet immediate priorities for the health sector as the fund could potentially be diverted to any other sector as well. The budget document also does not mention about this funding allocation which raises the question of whether, how, and which ministry or department will spend the money.
The current level of test, resource allocation, misappropriation of funds, fake testing, etc. indicate we are heading in the wrong direction. This is not a usual time. Bold decisions and strong political will are needed both in terms of allocation of resources and proper usage of funds. While the health sector is perhaps not the only sector to be blamed for poor management and under-performance, it is the most important sector to prioritise allocation, bring efficiency and transparency considering the pandemic. The current crisis offers an opportunity to address the bottlenecks of various sectors of the economy, and let's hope the health sector will be the first.
Asad Islam, Director, Centre for Development Economics and Sustainability (CDES) and professor, Department of Economics, Monash University, Australia. Hashibul Hassan, doctoral candidate, Monash University, Australia. Tabassum Rahman, doctoral candidate, Public Health and Behavioural Science, University of Newcastle, Australia.

 For all latest news, follow The Daily Star's Google News channel.
For all latest news, follow The Daily Star's Google News channel. 



Comments