Don’t let a ‘good crisis’ go to waste
The year 2020 was like no other in recent history. It saw, in the words of WHO Director-General Tedros Adhanom, a "once-in-a-century health crisis", referring to the Covid-19 pandemic, which continues to rage across the world. The 1918-20 Spanish flu, of course, dwarfed the current pandemic in terms of numbers, infecting a third of the world's population and killing about 50 million. Notwithstanding the hundred-year gap and the difference in magnitude, there are some remarkable similarities between the two pandemics in the way people reacted to them. For example, both saw resistance to masks and hygiene etiquettes. A group self-styled "Anti-Mask League" was active in 1919 in America's San Francisco; during the current pandemic, salespersons in groceries and restaurants who demanded that customers wear masks were attacked.
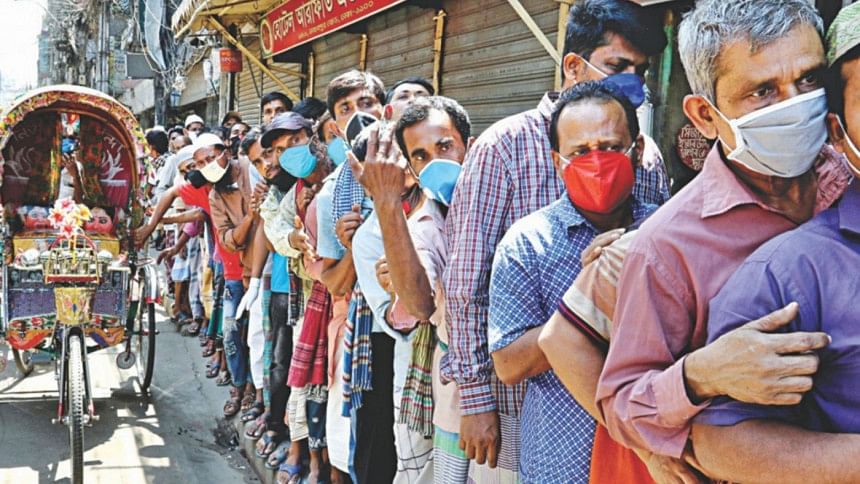
In Bangladesh, we have noticed a lack of enthusiasm to wear masks among a section of the public. Fortunately, we are yet to hear of any organised opposition or resistance to it as seen in other parts of the world. Bangladeshis are known for easily adapting to new ideas when convinced. We have seen this time and again. But the key is, they have to be "convinced". This requires special attention and deliberate organised efforts, similar to ones we have seen in cases of family planning, immunisations or oral rehydration therapy (ORT). Typically, such efforts come from the public sector. In specific cases, non-governmental sectors also played critical roles.
Introducing new concepts is always tricky but if done diligently and patiently, it usually comes to fruition. In the 1980s, BRAC implemented a nation-wide programme to popularise the use of ORT for treating the scourge of diarrhoea. Of the twin challenges of transferring the technology to mothers and making them use it, the former was found to be rather easier. With careful planning and house-to-house visits across the country, BRAC was able to transmit the message of how to make the diarrhoea solution correctly. But making people use it was an entirely different ball game. Initial research pointed to a very low utilisation rate—10 percent. BRAC mounted a research programme to understand why this was happening, even when knowledge surrounding the benefits of ORT was nearly universal. The information retrieved through the research was then used to modify BRAC's approach to programme implementation.
One of the reasons found, for example, was the lack of involvement of men in the programme. The health workers were all women, who connected with the women in the villages, keeping the men uninformed. This often led to speculations and suspicions about the "real" motive of the BRAC programme. In our society, men are often the decision makers and keeping them in the dark meant that women lacked the agency to use the solution. BRAC augmented its strategy by recruiting male workers and connecting with the men at bazars, mosques, temples, schools and tea stalls. It, along with other modifications, worked. The use rate climbed over time and Bangladesh now has the highest use rate of ORT in the world, with over 80 percent of mothers using it when their children have diarrhoea. Not only this, the concept of ORT is now being transmitted intergenerationally.
Coming back to the current pandemic, we are struggling with the use of masks. Are we approaching this problem keeping the twin challenges in mind? To date, I am not aware of any scientific study that examined the reasons why people are reluctant to use masks. The world is celebrating the arrival of vaccines now. There are still many questions to be answered about these vaccines in terms of their availability, duration of immunity, logistics and financing. For a country like ours, it may be "Dilli dur ast"—still a long way to go. Until we are able to vaccinate the majority of our population and create the so-called herd immunity, masks and hygiene etiquettes will remain our only armour against the virus. The government and the society as a whole haven't done enough in this respect yet.
Despite grave predictions, Covid-19 has not appeared as the greatest crisis in the history of Bangladesh. Indeed, compared to many others, we have been able to carry on. The Bloomberg report that included us in the league of 20 most resilient nations fighting the pandemic is a testimony to this, and we are proud of that. Given the resilience of the people, perhaps we could do better if right policies were adopted and implemented well.
The decade following the end of the Spanish flu saw unprecedented progress in the USA. As The Economist said recently, "the Roaring Twenties became a ferment of forward-looking, risk-taking social, industrial and artistic novelty." The Spanish flu also led to qualitative change in the ways medical practice and education are conducted. More than half of the medical schools were closed down due to poor quality. The new discipline of public health made its debut with the opening of the Johns Hopkins Bloomberg School of Public Health, thanks to the far-sighted philanthropists such as the Rockefellers.
As the saying goes, "never let a good crisis go to waste". This necessitates acting quickly and decisively to mitigate the crisis in a way that demonstrably impacts people's lives. The Covid-19 crisis has revealed the weaknesses in Bangladesh's health system. These include inadequate surveillance systems and capacity to track the spread of the virus, shortages of health human resources of all categories, lack of essential facilities and equipment (e.g. functioning primary care centres, hospitals and ICUs), insufficient specialised equipment (ventilators, testing kits and PPEs) and supply of necessary drugs. Unlike other natural disasters in the past, we have been overwhelmed in this particular case. The head of the government firmly took over the helm but others seemed ill-prepared, leading to poor or little coordination between the different arms of the state. Efforts to get citizens on board were tragically absent. It also showed how poverty and vulnerability deterred enforcement of tough actions in protecting citizens' health. Added to this is the inherent crisis of valid, relevant and timely data.
Covid-19 has set the ground for a "new" health system. Bangladesh has about 30-40 million people who are poor by any standard. With rising poverty and unemployment due to the crisis, this number is likely to rise to about 50 million in the next two to three years. They, in addition to the remaining population, will need publicly financed healthcare. With such a deadly disease ever-present amongst us, with the potential to flare up quickly, it is in our best interest that there is truly universal access to a full range of health services needed to tackle the disease and other conditions. Covid-19 is, therefore, perhaps the ultimate example of why we need universal health coverage (UHC)—if anyone is left out, it threatens the health security of everyone.
The government led by Prime Minister Sheikh Hasina has committed to achieve UHC for Bangladesh. Unfortunately, this commitment remains unimplemented. But perhaps the Covid-19 crisis and its aftermath might give the government the impetus to bring universal healthcare to everyone in the country. The government spends less than 1 percent of the nation's GDP on health, the lowest in the world. Our South Asian neighbour Sri Lanka, for example, spends four times as much. Seventy-four percent of our nation's health expenditures are borne out of pocket, leading 3-4 million people sliding into poverty every year. This will inevitably increase as a result of the Covid-19 fallout. The generous allocation of new resources to meet the pandemic-related challenges convinces us that the government, if committed, can make more money available for health.
The key to achieving UHC is reforming the health financing system. In particular, it requires switching from a system of private voluntary financing (mostly people paying fees for services) to a compulsory public system. This has happened in every developed country in the world. Many countries at Bangladesh's income level have made tremendous progress towards UHC including Sri Lanka, the Philippines, Vietnam and Morocco. Thailand achieved UHC in 2002 when its GDP per capita was almost exactly the same as Bangladesh's today. UHC is, therefore, perfectly affordable in Bangladesh.
Progressive leaders often take this initiative because UHC reforms are extremely popular. Across the world, politicians who have delivered UHC to their people have become national heroes. This was the case in Germany, France, Australia, Japan, Canada, Korea, Thailand, Brazil, Mexico, and Indonesia. It is also interesting to note how many of these great UHC reforms emerged out of national crises—including in the UK, France and Japan after WWII, Thailand in 2001 after the Asian financial crisis, and Rwanda after the genocide in 1994. And yet again in 2020, we are seeing some leaders recognising the opportunity that Covid-19 might give them to launch popular UHC reforms, notably in Ireland and South Africa. The crisis even precipitated a change of government in the United States where the Democrats campaigned on a pro-UHC platform.
Bangladesh's prime minister has the political capital and courage to go for a big push on UHC. As there are sufficient resources available in the country to achieve this goal, there is no reason why she shouldn't become Bangladesh's national UHC hero and write her name in the history books. What a wonderful gift this would be during the Mujib Borsho and the golden jubilee year of Bangladesh's independence!
Mushtaque Chowdhury is Convener of Bangladesh Health Watch, with its secretariat located at the James P Grant School of Public Health. He was previously Vice-Chair of BRAC.

 For all latest news, follow The Daily Star's Google News channel.
For all latest news, follow The Daily Star's Google News channel. 



Comments