Climate change is making us sick

A day before the latest United Nations Climate Change Conference (COP27) began, a group of global experts convened by The Lancet published a report about the adverse health effects of climate change. Their conclusion was as jarring as it was straightforward: human health is at the mercy of fossil fuels.
Unfortunately, health remained at the bottom of the priority list at COP27. To be sure, some important health-focused conversations took place at the World Health Organization's side pavilion. These discussions were particularly timely, given the current surge of Covid-19, fueled by the newest Omicron subvariants, in Europe and the United States. But, beyond a blink-and-you-miss-it mention in the preamble, the COP27 declaration makes no substantive mention of the climate-health nexus.
It is a glaring omission. The connection between climate and health is deep and multifaceted. Consider, for example, how warming temperatures and unprecedented flooding have encouraged the spread of mosquitoes – carriers of diseases like dengue fever, malaria, and the Zika virus – well beyond their traditional breeding grounds. If nothing is done, Zika will threaten an additional 1.3 billion people by 2050, and dengue fever will affect a whopping 60 percent of the world's population by 2080.
Similarly, climate-driven migration and shrinking animal habitats increase the risk that viruses and bacteria will jump from animal hosts to humans – just as SARS-CoV-2, the virus that causes Covid-19, likely did. This makes another pandemic increasingly likely.
Global warming is also worsening air pollution and, in turn, chronic non-communicable diseases like asthma and chronic obstructive pulmonary disease. Arvind Kumar, who founded the Lung Care Foundation in Delhi, laments that practically everyone in India has the health profile of a smoker, simply because of air pollution. In fact, nearly 1.7 million Indians die every year from its effects.
The people most affected by these climate-related health issues have often done the least to create them. Many residents of Bangladesh, Mozambique, and Pakistan do not even own cars. Yet they are suffering from the floods, cyclones, and rising sea levels that have resulted from developed-country emissions.
Fortunately, key lessons from the pandemic response can help us tackle the health challenges that climate change raises. For starters, we need a revolution in data collection and analysis. Global systems to capture and share relevant data progressed significantly during the pandemic, but we are still using only a small share of the information generated. Worse, the data tend to be divided into siloes.
To get a more complete picture of the health effects of climate change, we must integrate clinical, epidemiological, and genomic data from health systems with diverse non-health data, including on weather patterns, wastewater surveillance, consumer behaviour, and even social media and mobility. New open-source platforms like Global.health are an important step in the right direction, but much more must be done.
Another lesson from the pandemic is that, to avoid slipping back into the cycle of panic and neglect, any resilience agenda requires sustainable financing. When Covid-19 emerged, scores of global actors – particularly in the arena of vaccines research – acted with unprecedented speed and coordination.
But while large amounts of funding supported short-term initiatives, not nearly enough investment has been channelled subsequently toward pandemic prevention and preparedness. Likewise, while governments have responded to some of the immediate dramatic effects of climate change, such as natural disasters, interventions to address the climate crisis remain meagre.
As a first step, world leaders should back the Bridgetown Agenda, which seeks to reform global finance for the twenty-first century, including by ensuring that it supports climate action and pandemic prevention. They should also take every opportunity to connect climate and health issues in international forums, including at this month's UN Biodiversity Conference in Montreal.
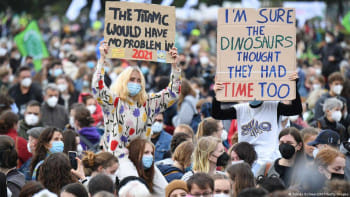
A final critical lesson from the Covid-19 pandemic is that an effective response depends on community trust and engagement. As with face masks and vaccines, community-based organisations and civil society will play a pivotal role in determining whether there is broad public buy-in for a bold agenda that covers both climate and health.
This will require a comprehensive, policy-shaping discussion that establishes a common language and shared intentions across sectors. Where should we aim to prevent the health consequences associated with climate change, and where should we mitigate them? Where should we adapt to the health effects of a warming planet, and why is an adaptation agenda becoming increasingly urgent?
In October, the UN confirmed that the world is far from meeting the goal, established in the 2015 Paris climate agreement, of limiting global warming to 1.5° Celsius above pre-industrial levels, and we may instead be headed to a catastrophic 2.8°C temperature rise by the end of the century. As the United Kingdom's COP27 representative Alok Sharma noted after the conference, the 1.5°C goal is now on "life support."
Concerted action must be taken to revive it – and that starts with recognising that climate and health are part of the same conversation. They can and must be tackled together.
Naveen Rao is Senior Vice President of the Health Initiative at The Rockefeller Foundation. Eloise Todd is Executive Director and Co-Founder of the Pandemic Action Network.
Copyright: Project Syndicate, 2022.
www.project-syndicate.org

 For all latest news, follow The Daily Star's Google News channel.
For all latest news, follow The Daily Star's Google News channel. 










Comments