Dengue prevention: What people and the government should do

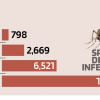
Bangladesh's dengue situation is critical, with one of the highest mortality rates in the world and the worst outbreak in history. This outbreak stems from the abundance of Aedes aegypti mosquitoes and the presence of the virus in human populations.
A study from 2014 to 2016 found that up to 85% of people in certain areas of Dhaka were seropositive for dengue. Typically, initial or multiple infections with the same dengue virus serotype pose no problem. However, infection with a different serotype later significantly increases the risk and complexity due to antibody-dependent enhancement, where antibodies against one serotype can worsen another. This can explain why there are so many severe dengue cases in Dhaka and other areas of the country. This year, for the first time, there are more dengue patients outside Dhaka, possibly due to an unprecedented abundance of Aedes aegypti mosquitoes in previously unaffected areas.
As the treatment is only symptomatic and there is a lack of accessible vaccines, the focus is on controlling the vector mosquitoes. However, the mosquito distribution has surpassed a level where the government's efforts alone are insufficient. We must take action ourselves.
Aedes aegypti, which I refer to as the household mosquito, largely depends on humans for blood meals and breeds close to or even inside our homes. Despite our familiarity with mosquito breeding sites like stagnant water or containers, there is a reluctance among people to take action. We must take responsibility for our homes and prevent mosquito larvae from growing in and around our living spaces.
In the fight against dengue, the government faces long-term challenges beyond their current efforts. Dengue cannot be eradicated overnight, and countries dealing with this issue offer valuable lessons. Since our 2019 recommendation, the use of malathion in the country is a positive step, but it is a short-term solution. Despite resource constraints, we can explore mosquito control methods.
The World Health Organisation recommends using 'Bendiocarb', an insecticide that is effective against Aedes mosquitoes, for indoor residual spraying. A recent success involves releasing Wolbachia bacteria to control Aedes mosquitoes and dengue. Wolbachia can significantly reduce dengue virus transmission, and if infected males mate with females, no larvae emerge. Research on introducing Wolbachia in Bangladesh is promising but needs further testing.
Comprehensive health education in schools through various media channels and strict laws for mosquito breeding site destruction are vital. In extreme cases, even a larva control programme may be necessary. I urge the government to provide substantial research support, as dengue remains a major threat to lives and the country's economy.
The writer associated with University of Queensland and QIMR Berghofer Medical Research Institute, Brisbane, Queensland, Australia.
E-mail: [email protected]

 For all latest news, follow The Daily Star's Google News channel.
For all latest news, follow The Daily Star's Google News channel. 






Comments