A Leading Cause of Death in Bangladesh
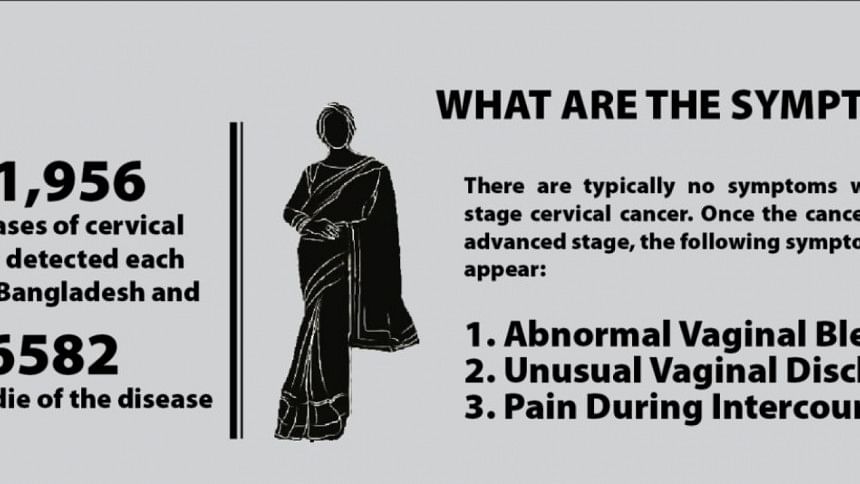
In Bangladesh, cervical cancer is the 2nd most common cancer in women. It is estimated that every year 11,956 new cases of cervical cancer are detected in Bangladesh and 6582 women die of the disease1.
The Cervix is the lower one third of the uterus. HPV (human papillomavirus) infection is a sexually transmitted disease and is the main cause for development of cervical pre-cancer and cancer. The high burden of cervical cancer in Bangladesh is possibly due to high prevalence of risk factors such as early marriage and young age at first birth, early initiation of sexual activity, high parity, sexually transmitted diseases and low socio-economic conditions. Women in Bangladesh demonstrate low awareness about cervical cancer, its symptoms, available screening and treatment options.
A comprehensive cervical cancer program requires government ownership and systematic management. It should include: HPV vaccination for girls; a population based cervical cancer screening program; an efficient referral system; availability of adequate healthcare providers and treatment equipment; a health financing option through universal health coverage; a population-based cancer registry, and as a last resort, improved and decentralized palliative care services.

Primary Prevention through Human Papillomavirus (HPV) Vaccination
HPV vaccination is primary prevention against cervical cancer and is given to girls before marriage. There is no national program for HPV vaccination in Bangladesh as of yet. Expanded Programme on Immunization (EPI) under the Directorate General of Health Services (DGHS) implemented a two-year HPV pilot project in Gazipur funded by GAVI, the Vaccine Alliance. It employed a school-based approach to vaccinate girls in grade 5; and a community-based approach to vaccinate 10-year old girls in community health facilities and vaccination centres. Girls were administered two doses in six-monthly intervals. Above 31,000 girls were vaccinated in 2016 (87% coverage) and 23,000 girls were vaccinated (coverage rate 99.67%) in 20172. Depending on the success of the project, the government plans to implement a national HPV vaccination program in 20193.
While HPV vaccination targets young girls, it is important to screen women of older age groups for cervical pre-cancer who require a mode of secondary prevention from cervical cancer.
Secondary Prevention through Cervical Cancer Screening
Screening for cervical precancerous lesions is form of secondary prevention. Dr. Ashrafunnessa, Professor, Department of Obstetrics and Gynaecology, Bangabandhu Sheikh Mujib Medical University (BSMMU) and Focal point of Cervical and Breast Cancer Screening Program described the program, "since 2004, the Government has developed a cervical and breast cancer screening program in all districts of Bangladesh through technical assistance of Bangabandhu Sheikh Mujib Medical University (BSMMU) and UNFPA. 411 centers have been established and about 1895 service providers trained on cervical screening (visual inspection with acetic acid, VIA) and breast cancer screening (clinical breast examination, CBE). 1386807 VIA tests were performed from 2005 to 2016 ,of which 65747 (4.74%) were found VIA-positive." This screening program has faced several challenges as well, namely: high drop-outs of women screened positive; high rate of staff turnover, which renders VIA centres void of a trained nurse to conduct VIA tests. Even though the current program has screened about a million women, the current opportunistic screening system will not be able to screen the national target population of 45 million women (who need to be screened at least once in their lifetimes if not every 5 years). The country needs to shift to an organized population based screening program to increase screening coverage.
Tertiary Prevention: Treatment and Management of Cervical Cancer
14 government medical college hospitals, along with BSMMU, have been developed as referral centers through development of colposcopy clinics with facilities for colposcopy, histopathology, and management of precancerous condition of the cervix. A recent review article summarized that nationwide that most oncology referrals are directed to public hospitals due to the high expense associated with private care. The Dhaka Medical College Hospital, National Institute for Cancer Research Hospital (NICRH) and BSMMU are overwhelmed by the influx of patients. However the number of trained oncologists and available radiotherapy machines are inadequate for the volume of patients, and are mostly urban-based.
Unmet Need for Palliative Care
Palliative care is an essential component of comprehensive cancer care. It provides end of life care to patients with terminal illness. Dr. Nezamuddin Ahmad Professor & Chairman Department of palliative Medicine Centre for Palliative Care at BSMMU stated "palliative care service remains an unmet need in the country; it is ignored in the mainstream health care service of the country and in government health policies. BSMMU established palliative care services in 2007, and transformed it into a Centre for Palliative Care (CPC) in 2011. Though cancer cervix remains the second most prevalent cancer in females, CPC offered its service to only 190 patients with cervical cancer since 2007- indicating that women with terminal cervical cancer are not seeking palliative care."
The need for a Population-Based Cancer Registry
Dr. Habibullah Talukder, Associate Professor and Head, Department of Cancer Epidemiology, National Institute of Cancer Research and Hospital described that "a well designed cancer control plan can only be developed and implemented with reliable and valid statistics of incidence and prevalence of cancer, ideally provided through population- based cancer registries (PBCR), which collects data on all new cases of cancer occurring in a well defined population. Additionally, Nabila Hossain Purno, Research Associate at UNFPA, Bangladesh mentioned that "there is a huge need for implementation and epidemiologic research to better understand existing challenges and provide solutions to increase uptake of screening, reduce loss to follow up and track patient flow within the system for cervical cancer".
Improvement in Cervical Cancer Care will help to achieve Gender Equality and the SDGs
Dr. Sathyanarayanan Doraiswamy, Chief Health, UNFPA Bangladesh, stated that "mortality from cervical cancer is lowest where the health systems are more gender equitable, placing the health and rights of women and girls at its core". Advances in cervical cancer care will help Bangladesh achieve both Sustainable Development Goals 3 (Ensure healthy lives and promote wellbeing for all at all ages) and 5 (Achieve Gender Equality and and empower all women and girls).
The Way Forward
Currently, the Government is finalizing the national cervical cancer strategy (2017-2022), which aims to provide technical and strategic guidance in developing a comprehensive cervical cancer control plan. Cervical cancer will strain the country's public health resources catastrophically if the healthcare system doesn't prepare for systematic management of cervical cancer prevention and control.
Technical and clinical experts as well as the global evidence provide the following recommendations:
♦ Implementation of a national HPV vaccination program for vaccinating girls of target age group
♦ Gradually implement an organized population based cervical cancer screening program instead of the current opportunistic system.
♦ Develop decentralized national cervical cancer training and treatment centres, which are well equipped with diagnostic and treatment machines, including adequately trained health care providers.
♦ Establish a population based cancer registry to record data on cancer incidence, prevalence and trends.
♦ Improved focus and resource allocation to decentralized palliative care systems for terminal cervical cancer patients.
The article is prepared by UNFPA Bangladesh Country Office.
Reference:
1. Human Papillomavirus and Related Diseases Report, Bangladesh; ICO Information Centre on HPV and Cancer, 2017
2. Coverage Evaluation Survey, 2016 & 2017, Expanded Programme on Immunization
3. Dr. Md. Jahangir Alam Sarker Director, DGHS and Line Director, MNC&AH; Dr. Md. Altaf Hossain Program Manager, EPI, DGHS; and Dr. Mohammad Zahid Haider Medical Officer, EPI & Surveillance, DGHS

 For all latest news, follow The Daily Star's Google News channel.
For all latest news, follow The Daily Star's Google News channel. 



Comments