Dengue deaths cross 200
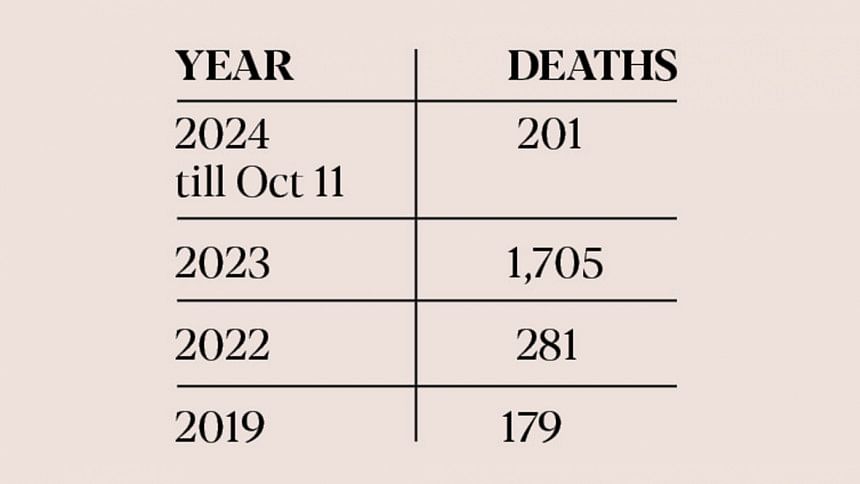
With two more dengue deaths reported yesterday, the total number of fatalities from the disease this year has risen to 201, making it the third-highest death toll since the outbreak in 2000.
According to the Directorate General of Health Services, 1,705 dengue deaths occurred in 2023, marking the highest annual death toll to date. In comparison, there were 281 deaths in 2022 and 179 in 2019.
The total number of recorded dengue cases this year has reached 40,895 as of yesterday.
Experts attribute the high mortality rate this year to factors including late hospitalisation, quick onset of shock syndrome, inaccurate test results, and recurrent dengue infections.
Dr HM Nazmul Ahsan, associate professor at Shaheed Suhrawardy Medical College Hospital, said, "Many patients are going into shock right after their fever subsides, which is very alarming."
Dr Ahsan further noted the large number of patients presenting with shock syndrome, bleeding, and expanded dengue syndrome, which has contributed to the rising death toll. He urged all to stay vigilant and seek medical attention at the first sign of warning symptoms, as early intervention can significantly reduce the risk of death.
Shock syndrome in dengue patients can be classified into two categories: compensated shock and decompensated shock. In compensated shock, a patient's blood pressure may appear normal or slightly low, but with a dangerously narrow pulse pressure (less than 20). Decompensated shock, however, is more severe, involving symptoms such as disorientation, cold and clammy skin, unrecordable blood pressure and pulse, and an inability to urinate.
"Patients experiencing decompensated shock can die within minutes," Dr Nazmul said.
He also highlighted that high-risk groups, including the elderly, obese individuals, pregnant women, infants, and people with comorbidities, are more susceptible to fatal outcomes.
Dr Ahsan advised that severe stomach pain, difficulty breathing, extreme weakness, bleeding from the gums or nose, and vomiting should be treated as signs for immediate hospitalisation. "Failure to hospitalise patients showing these warning signs can result in shock syndrome," he added.
While patients in compensated shock can recover with prompt treatment, those in decompensated shock face a survival rate of only 50 percent.
Dr Ahsan said in many cases, faulty test kits produce false results, causing patients to seek hospital care only when their condition has already worsened. He recommended consulting a doctor immediately after developing a fever and performing a Complete Blood Count (CBC) test on the third or fourth day of fever, even if the NS1 test for dengue is negative.
Public health expert Mushtaq Hussain emphasised the need for changes in treatment strategies to reduce the mortality rate. He suggested the government divide care into three levels -- primary, secondary, and tertiary -- to streamline patient management and lower death rates.
He said a stronger primary healthcare system is essential as many people lack access to dengue testing at local clinics. This leads to late diagnoses, especially for impoverished communities.
Mushtaq also proposed establishing additional blood collection centres and expanding secondary care facilities in the city to reduce the burden on medical college hospitals.
"City corporation and railway hospitals could be used for secondary care, with critical patients transferred to medical colleges when necessary," he said.

 For all latest news, follow The Daily Star's Google News channel.
For all latest news, follow The Daily Star's Google News channel. 



Comments