Antibiotics Overuse: Headed for a health calamity
Almost all clinically important and widely used antibiotics have lost their effectiveness by more than 50 percent, found a recent study -- a development that can leave the population defenceless against pandemics.
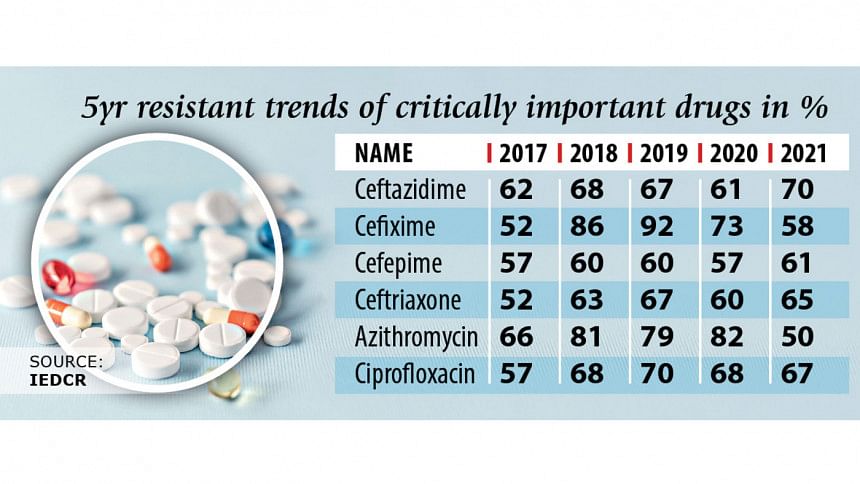
Most worryingly, five of the most critical medicines listed by the World Health Organisation are progressively becoming ineffective, according to the surveillance study by the Institute of Epidemiology, Disease Control and Research conducted between 2017 and 2021.
"The message of this study is that the situation is alarming," said Meerjady Sabrina Flora, additional director general of the health directorate, at an event yesterday to unveil the performance of 21 antibiotics against 10 priority pathogens.
The drugs were tested against bacteria responsible for diseases such as urinary tract infection, septicaemia, diarrhoea, pneumonia and wound infection, among others.
The study, which was conducted in nine medical college hospitals, found 9 percent of the examined bacteria was resistant to all available antibiotics.
The ineffectiveness of antibiotics to kill microorganisms like bacteria, viruses and parasites is called antimicrobial resistance (AMR).
"The AMR is another type of pandemic. It should not be that there is no drug for curing illnesses," Flora said.
Data indicates that the use of antibiotics is driven by practitioners, said Nitish Chandra Debnath, One Health Bangladesh's national coordinator.
"We have to work on it -- we need a strong movement among professionals. AMR is a challenge for both the public health and the economy," he added.
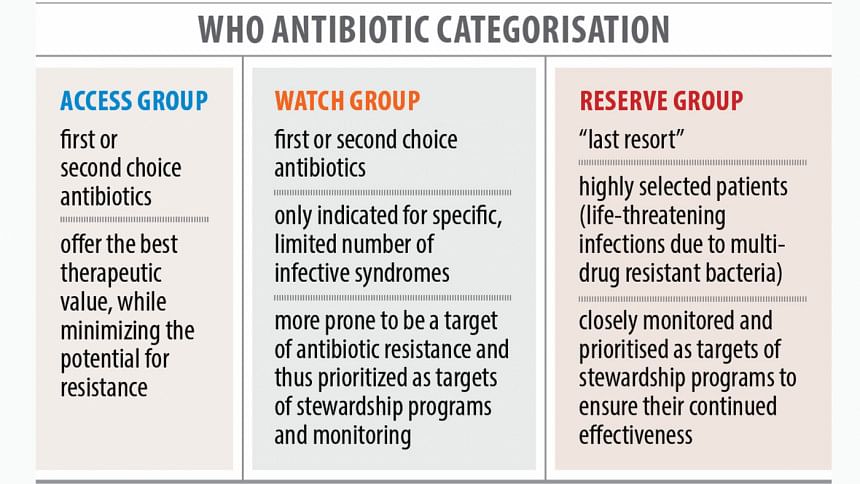
Antibiotics are classified into three sets: the "access group" is prescribed for a wide range of primary level infections, the "watch group" for higher resistance bacteria and the "reserve group" when all alternatives fail.
Of the 21 antibiotics, seven were from the access group, nine from the watch group and two from the reserve group. Of them, 15 are progressively becoming ineffectual.
In 2021, Ceftazidime, a watch group drug, has become ineffective in killing different bacteria in 70 percent of the cases. In 2017, its ineffectiveness rate was 62 percent.
The ineffectiveness has increased from 52 percent to 58 percent for Cefixime, from 57 percent to 61 percent for Cefepime, from 52 percent to 65 percent for Ceftriaxone, from 57 percent to 67 percent for Ciprofloxacin, from 20 percent to 40 percent for Carbapenem. All are watch group drugs.
During the period, access group drugs Doxycycline and Tetracycline have become more useful, with their ineffectiveness rates decreasing from 47 percent to 39 percent and from 58 to 54 percent respectively.
"This may be because of the lesser use of these drugs -- physicians mainly use drugs from the watch and reserve groups," Zakir Hossain Habib, lead investigator and head of microbiology at the IEDCR, told The Daily Star.
Among the access group, drugs that have lost effectiveness include Nitrofurantoin, Sulphamethoxazole-Trimethoprim, Ampicillin, Amoxicillin-Clavulanate and Gentamicin. Penicillin have slightly gained in effectiveness.
The ineffectiveness of Aztreonam, a reserve group drug, has increased to 61 percent from 59 percent; it has remained static at 37 percent in the case of reserve group drug Linezolid.
"We are losing our first-line antibiotics [access group] -- the second-and third-line antibiotics are costly and toxic," said Mohamed Ramzy Ismail, WHO technical expert on essential drugs and medicines in Bangladesh.
There are only a few promising options for new antimicrobials in the research pipeline, he said.
To fight AMR, Ismail called for the "One Health" approach, where Bangladesh has made good progress.
One health recognises that human health is closely connected to the health of animals and the shared environment.
Some countries are using antibiotics more in food production than in medical care.
"We need to find ways to target all behaviour that contribute to the misuse of these fragile medicines," he added.

 For all latest news, follow The Daily Star's Google News channel.
For all latest news, follow The Daily Star's Google News channel. 



Comments