Develop a patient referral system

It is unfortunate that 53 years since independence, we have failed to develop a functional referral system, with a staggering three out of five patients directly referring themselves to specialists and tertiary hospitals, according to a recent study. This inevitably overwhelms tertiary facilities, leads to long waits, and deprives critically-ill patients of due attention and care. Unlike in countries such as the UK, where patients are required to see a general practitioner before being referred to a specialist, it is common practice in Bangladesh for patients to directly visit specialists even for minor ailments. This has created a lop-sided system, where the tertiary hospitals bear an overwhelming brunt of the pressure, while primary and secondary facilities remain underutilised and underdeveloped.
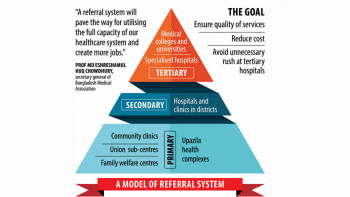
A well-designed referral system can help streamline the healthcare network, and create an effective linkage among three tiers of healthcare services. Primary healthcare facilities, which should be the first point of contact for any patient, should be fully equipped to take care of basic cases, referring only the complex cases to specialists. A 2023 study found that a referral system can filter as many as 65 percent of patients at primary and secondary healthcare facilities at upazila and district levels, freeing up tertiary facilities to focus on their core functions. Given the obvious advantages of such a system, the question is: why have we not implemented this system so far?
What is obvious is that ad hoc attempts at implementation will not work without a radical reimagining of the healthcare system and appropriate investments and capacity-building to ensure a successful transition.
There have been various discussions over the decades about instituting such a system, but previous attempts to implement it have stumbled for various reasons. A referral system for Rangpur was announced in 2014 by the then health minister Mohammad Nasim, but it failed as a result of inadequate logistical support and unavailability of qualified physicians and auxiliary workforce at primary healthcare centres. Attempts to get the system going in 2016 and 2019 also fizzled out in the end. What is obvious is that ad hoc attempts at implementation will not work without a radical reimagining of the healthcare system and appropriate investments and capacity-building to ensure a successful transition.
The good news is that Bangladesh already has primary healthcare infrastructure in rural areas, with community hospitals and community clinics, but their systemic issues—shortage of staff, equipment and inefficiencies in operations—need to be addressed if they are to play their due role within the referral system. Meanwhile, tertiary facilities have mushroomed in urban areas at the cost of primary and secondary facilities—an imbalance that must first be addressed.
If we are to move forward, we need political will and a well-defined policy about how to implement a well-designed referral system. The system must be built on a strong foundation of well-equipped primary healthcare facilities, a sufficient number of trained specialists at all levels, and a public that trusts and understands the system.

 For all latest news, follow The Daily Star's Google News channel.
For all latest news, follow The Daily Star's Google News channel. 









Comments