Want to beat bone loss? Change your lifestyle!
When frequent painkillers stopped bringing much relief, Radhika Saha went to see a doctor for severe back pain. That was when she found out her bones were weakening, and that if they were not taken care of, the symptoms might lead to fracture.
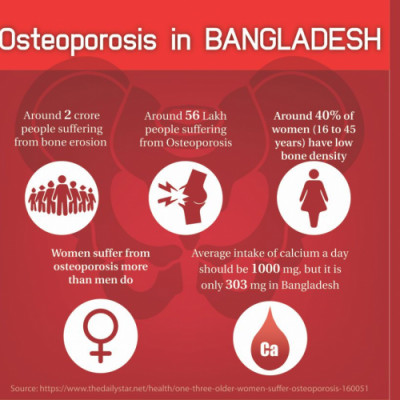
Losing bone mass is defined as osteoporosis (meaning porous bone). Like 60-year-old Radhika, women are more likely than men to suffer early from the disease as a result of post-menopausal health complications.
Immediate medical attention and change in lifestyle can delay or slow down the process of reduction in bone mass and strength whereas a lack of awareness among doctors and patients causes most cases to remain undiagnosed in the country until it is too late, according to experts. There are preventive measures as well like including milk and dairy products in everyday diet, regular exercise and enough exposure to sunlight for the body to produce vitamin D.
Osteoporosis is a gradual decrease in bone density and so the symptoms—pain around the wrist, lower spine and hip—appear long after one begins losing bone mass.
Everyone suffers from the disease sooner or later as he or she ages, said Arun Kumar Sarker, assistant professor of orthopaedics at the National Institute of Traumatology and Orthopaedic Rehabilitation (Nitor) in the capital. People should be made aware of this so it can be controlled and so that they can avoid pain, fracture and fracture-inflicted death.
Globally, one in three women and one in five men over the age of 50 will have an osteoporosis-related fracture in their lifetime.
In this country, people from lower socioeconomic strata are thought to suffer more from osteoporosis and osteoporosis-related fracture owing to poor nutritional diets and their inability to afford medical care.
An inactive lifestyle and less exposure to sunlight are major factors behind the loss of bone mass among people belonging to middle and upper classes. And a lack of knowledge about treatment opportunities leaves them crippled even though the health issue is treatable.
No research has been done yet to find out the severity of the problem across different strata of the population here, but the problem seems to be severe if we go by the experiences of handling outpatients in hospitals, said Prof Syed Atiqul Haq, chairman of the medicine department at Bangabandhu Sheikh Mujib Medical University.
Eight out of 10 patients whom he has come across have been diagnosed with osteoporosis when subjected to the bone mineral density (BMD) test, an efficient but expensive way to confirm the disease.
Most of the patients who receive healthcare at public hospitals are middle-class, said Mr Haq. “The conditions of the poor and the disadvantaged are obscure.”
All women aged above 65 and men above 70 should take the BMD tests, regardless of whether there are any signs of osteoporosis, to learn about their bone health, Mr Sarker said. That would help them take precautionary measures like increasing their calcium intake or receiving necessary medication.
Often doctors prescribe medication looking at symptoms only— without taking the test that costs at least Tk 3,000 because most patients would consider it as an unnecessary burden before the treatment even begins, he said. Also, a very few healthcare facilities offer such tests.
When diagnosis and treatment costs are matters of concern, the need for addressing the skeletal disease is imperative. By 2050, the population pyramid will change with a swelling elderly population replacing today’s young population.
The government can play a significant role. It can bridge the gap by ensuring the needed infrastructure and the number of specialised physicians required to provide treatment to a greater population.
It can also create awareness and take measures paying heed to the special nutritional needs to keep osteoporosis at bay, said Mr Haq. For example, “The government can issue a directive that milk cannot be sold unless fortified with vitamin D” as is the case of salt with iodine.


 For all latest news, follow The Daily Star's Google News channel.
For all latest news, follow The Daily Star's Google News channel. 



Comments